We combine entity and policy data with vast 3rd party data to give insurers a clearer picture of the entities, inputs, and influences on every transaction.
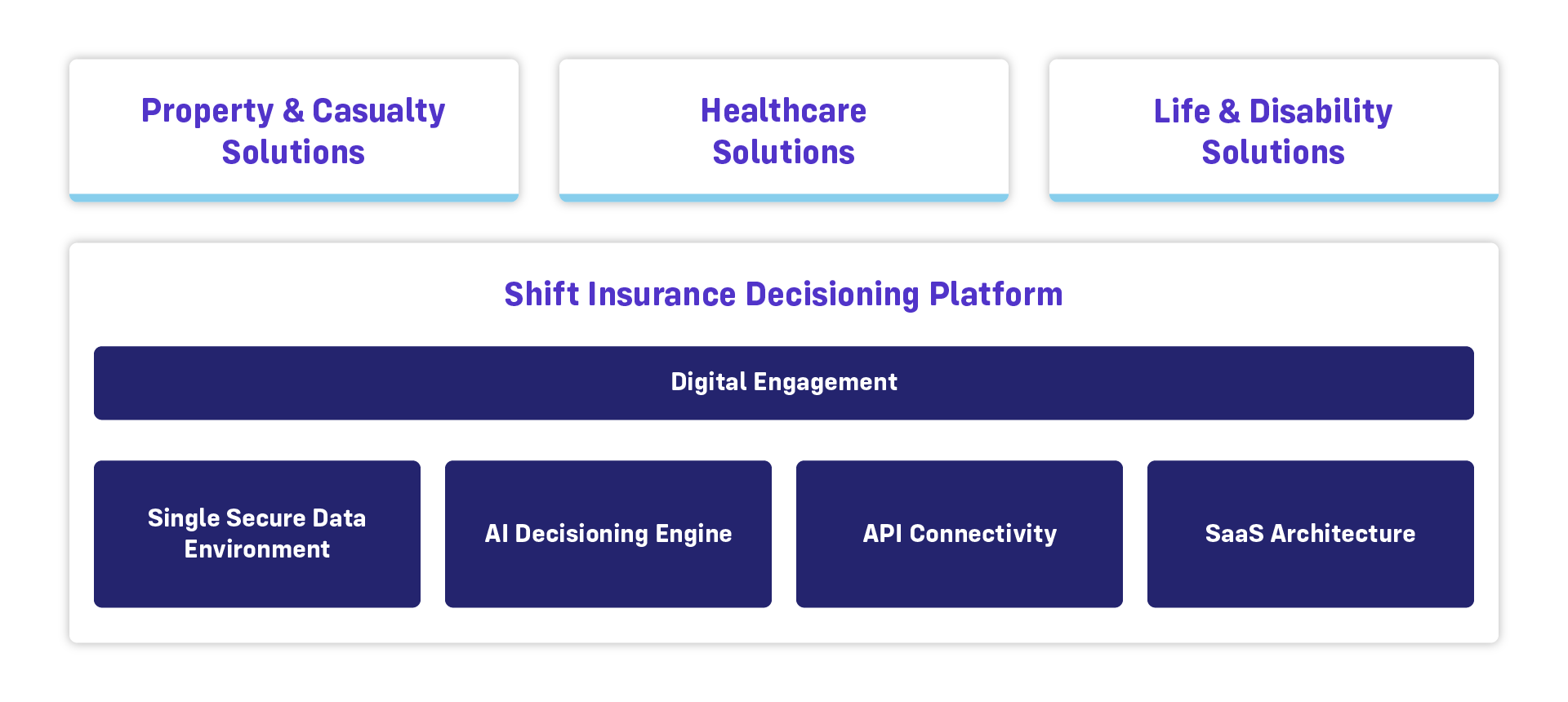
The Shift Insurance Decisioning Platform
Enable greater speed and accuracy in decisions throughout the policy lifecycle
Better Decision-Making Starts Here
The Shift Insurance Decision Platform is a unified software architecture designed to improve insurance decisions across the entire claims lifecycle. The platform uses artificial intelligence to enhance claims decisions at multiple touchpoints, including intake, fraud detection, subrogation, and more. This eliminates bottlenecks from the claims lifecycle, yielding faster, fairer, and more accurate decisions.
- Acts as an AI-enabled "decisioning layer" that integrates with insurer core systems via API
- Combined internal insurer data with 3rd party data to deliver unmatched insights
- Delivers ROI throughout the policy lifecycle
- Supported by the largest team of insurance-focused Data Scientists in the world
Impact:
Provides accurate, data-driven decision guidance and significant automation of both routine and complex tasks
Data driven insights and automated decisioning increase insurers' capacity and accuracy while enabling new initiatives.
Liberate resources to focus on what matters most: the policyholder or member. Better decision-making frees insurers to be there for their customers.
The Shift Insurance Decisioning Platform